مقدمة: When Light Becomes Medicine
Imagine a treatment that requires no medication, غير الغازية وغير مؤلمة, ويستخدم أطوال موجية محددة من الضوء لتسريع التئام الجروح. هذا يبدو وكأنه خيال علمي, ولكنها حقيقة أثبتها الطب الحديث. العلاج بالضوء الأحمر, كان يعتبر في السابق علاجًا بديلاً هامشيًا, is now entering the mainstream medical field with solid scientific evidence. The global wound care market is expected to reach $28.5 billion by 2027, and photobiomodulation, as one of its fastest-growing segments, is changing our understanding of wound treatment.
Chapter 1: What Exactly is Red Light Therapy?
Definition and Historical Development
العلاج بالضوء الأحمر, scientifically known as “photobiomodulation” أو “العلاج بالضوء منخفض المستوى,” is a treatment method that uses specific wavelengths of red light (630-700 نانومتر) والأشعة تحت الحمراء القريبة (700-1100 نانومتر) to deliver non-thermal, low-energy irradiation to biological tissues.
The origin of this technology dates back to 1967, when Hungarian scientist Endre Mester accidentally discovered that low-power laser light stimulated hair regrowth and wound healing in mice. This accidental discovery opened the door to photobiomodulation research. Over several decades, أكثر من 4,000 clinical studies gradually revealed its mechanisms of action, moving it from the laboratory to clinical practice.
The Fundamental Difference from Ordinary Light
Red light therapy is fundamentally different from ordinary lighting or sunbathing:
- Precise Wavelength: Uses only specific light in the 600-900 nanometer band.
- Low-Energy Characteristic: Power density typically ranges from 5-500 milliwatts per square centimeter, only 1/100th to 1/1000th of laser therapy.
- Non-Thermal Effect: Does not produce a noticeable sensation of heat during treatment; works through photochemical rather than thermal effects.
- Specific Wavelength Action: Different wavelengths penetrate to different depths and target different areas; red light acts on more superficial layers, while near-infrared light reaches deeper tissues.
Chapter 2: In-Depth Analysis of the Scientific Principles
Cellular-Level Mechanisms: How are Mitochondria “Activated”?
The core action of red light therapy occurs within the mitochondria—the cell’s “power plants.” السيتوكروم ج أوكسيديز (CCO) in the inner mitochondrial membrane is the primary absorber of photons, known as the “photoreceptor.”
Molecular Cascade of Photobiomodulation:
- Photon Absorption: Photons with wavelengths of 600-900 nanometers are absorbed by CCO.
- Enzymatic Activity Change: The conformation of CCO changes, increasing enzymatic activity by 30-40%.
- ATP Production Surge: Adenosine triphosphate (ATP)—the cell’s energy currency—production increases by 50-150%.
- Signal Cascade Initiation: Increased ATP triggers downstream signaling pathways, مشتمل:
- A brief, moderate increase in reactive oxygen species (روس) as signaling molecules.
- Activation of transcription factors (such as NF-κB).
- Changes in gene expression, promoting the synthesis of repair-related proteins.
Specific Impact on the Four Stages of Wound Healing
Wound healing is a meticulously orchestrated biological process, and red light therapy plays a unique role in each stage:
1. Hemostasis Phase (Immediately After Injury)
- Enhances platelet activity and promotes the release of clotting factors.
- Accelerates vasoconstriction, reducing initial blood loss.
2. Inflammatory Phase (أيام 1-3 Post-Injury)
- Modulates Rather Than Suppresses Inflammation: Moderately reduces pro-inflammatory factors (TNF-α, إيل-1β) and increases anti-inflammatory factors (IL-10).
- Accelerates the clearance of debris and pathogens by neutrophils and macrophages.
- Prevents chronic inflammation, a key reason why chronic wounds fail to heal.
3. Proliferative Phase (أيام 3-21 Post-Injury)
- Accelerates Fibroblast Proliferation by 40-60%: These cells are the primary producers of collagen.
- Increased Collagen Synthesis: Synthesis of Type I and Type III collagen increases by 50-70%.
- Enhanced Angiogenesis: Increased expression of vascular endothelial growth factor (VEGF) promotes new blood vessel formation.
- Accelerated Epithelialization: Keratinocyte migration speed improves by 30-50%.
4. Remodeling Phase (21 Days to 1 Year Post-Injury)
- Improves collagen alignment and reduces scar formation.
- Enhances the mechanical strength of new tissue.
Key Supporting Research Data
- أ 2018 meta-analysis published in Wound Repair and Regeneration showed that red light therapy increased the complete healing rate of chronic wounds by 32% (relative risk 1.32, 95% CI 1.15-1.51).
- In studies on diabetic foot ulcers, patients receiving red light therapy had an average healing time shortened by 21.4 أيام.
- A randomized controlled trial on pressure ulcers found that the healing speed in the red light treatment group was 2.1 times faster than that of the control group.
Chapter 3: Which Wounds Are Most Suitable for Red Light Therapy?
Highly Responsive Wound Types
1. Chronic, Hard-to-Heal Wounds (Strongest Clinical Evidence)
- تقرحات القدم السكرية: Systematic reviews show that when combined with standard care, the complete healing rate increases from 34% ل 52%.
- Pressure Ulcers (Bedsores): The rate of area reduction for Stage II-IV pressure ulcers improves by 40-60%.
- Venous Leg Ulcers: Particularly effective for patients with a duration of illness exceeding 6 شهور.
2. Acute Wounds
- Surgical Incisions: Reduces postoperative pain and swelling, lowers infection risk, and results in more aesthetically pleasing scars.
- بيرنز: Healing time for superficial second-degree burns is shortened by an average of 3-5 أيام, with reduced pain scores.
- Abrasions and Lacerations: Accelerates the epithelialization process and reduces scabbing time.
3. Other Indications
- Radiation dermatitis (skin damage after cancer radiotherapy).
- Post-herpetic skin lesions.
- Hidradenitis suppurativa wounds.
Wound Types with Limited Effectiveness
- Ischemic wounds (severely insufficient blood flow).
- Wounds covered with necrotic tissue that has not been debrided.
- Wounds associated with malignant tumors.
Chapter 4: Clinical and Home Use Guidelines
Medical-Grade Treatment Parameters
In professional medical settings, doctors adjust parameters based on the wound type:
| Wound Type | Recommended Wavelength | Energy Density | تكرار | Treatment Cycle |
|---|---|---|---|---|
| Diabetic Foot Ulcer | 660نانومتر + 850nm combination | 4-6 ي/سم² | 2-3 مرات في الأسبوع | 8-12 أسابيع |
| Stage II-III Pressure Ulcer | 630-660نانومتر الضوء الأحمر | 3-4 ي/سم² | Daily or every other day | 4-8 أسابيع |
| Surgical Incision | 810-830نانومتر بالقرب من الأشعة تحت الحمراء | 2-3 ي/سم² | Daily for 3-5 consecutive days post-op | Single course |
| Superficial II-Degree Burn | 630نانومتر الضوء الأحمر | 1-2 ي/سم² | Once daily | 7-10 أيام |
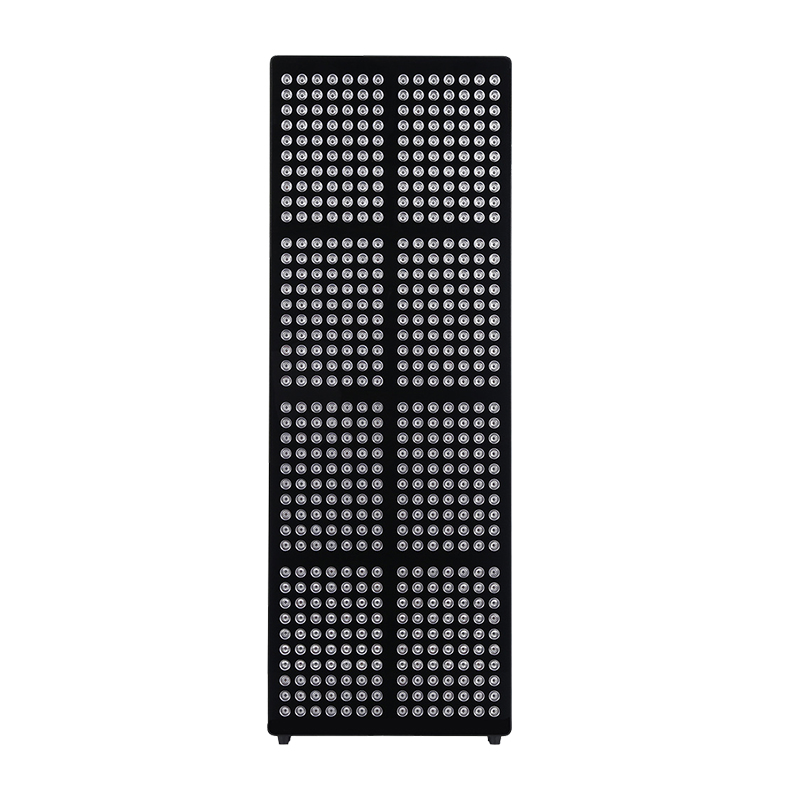
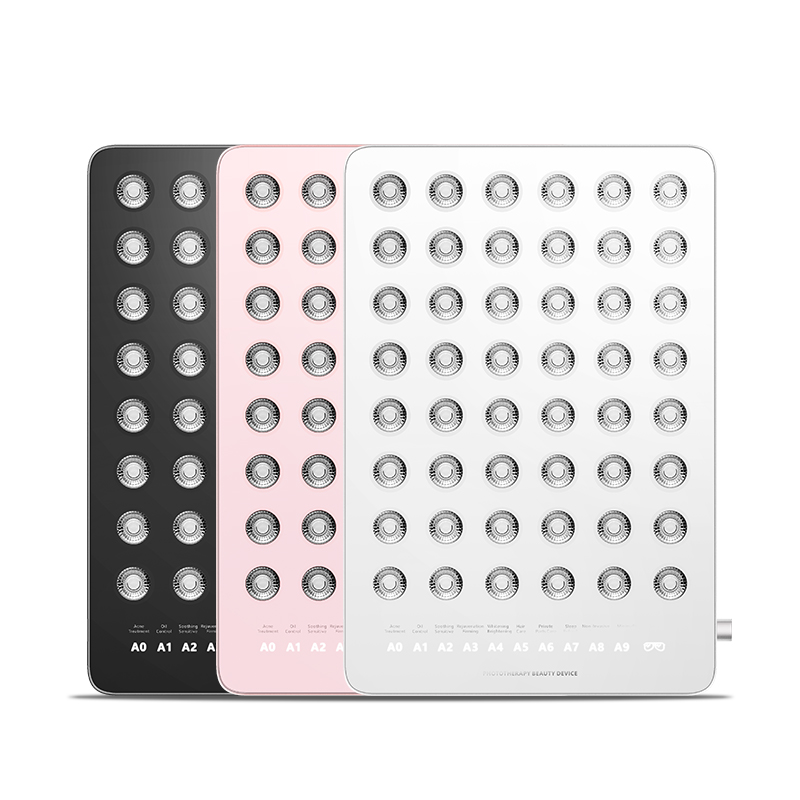
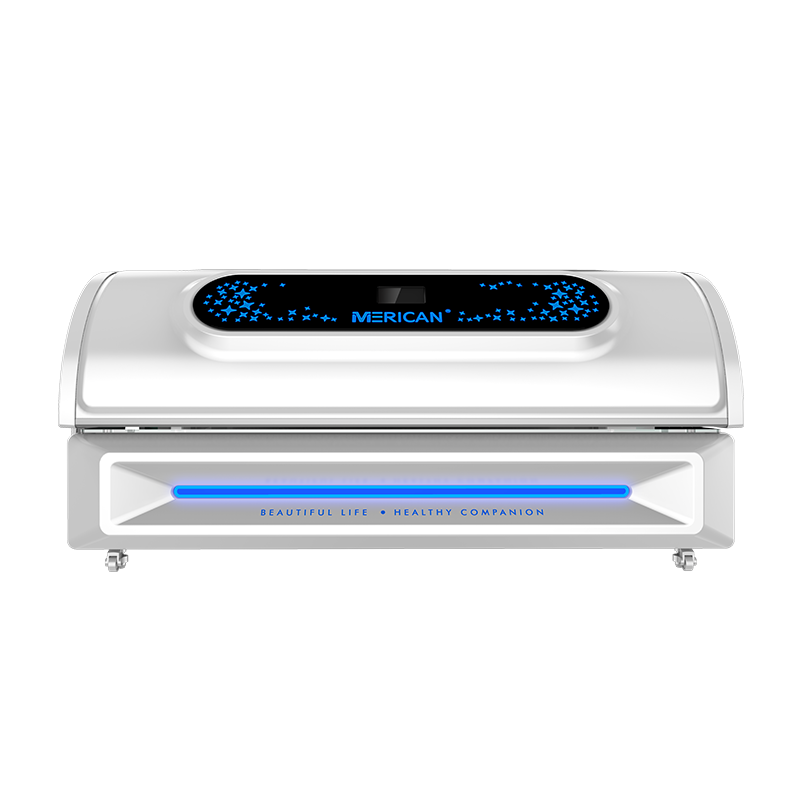
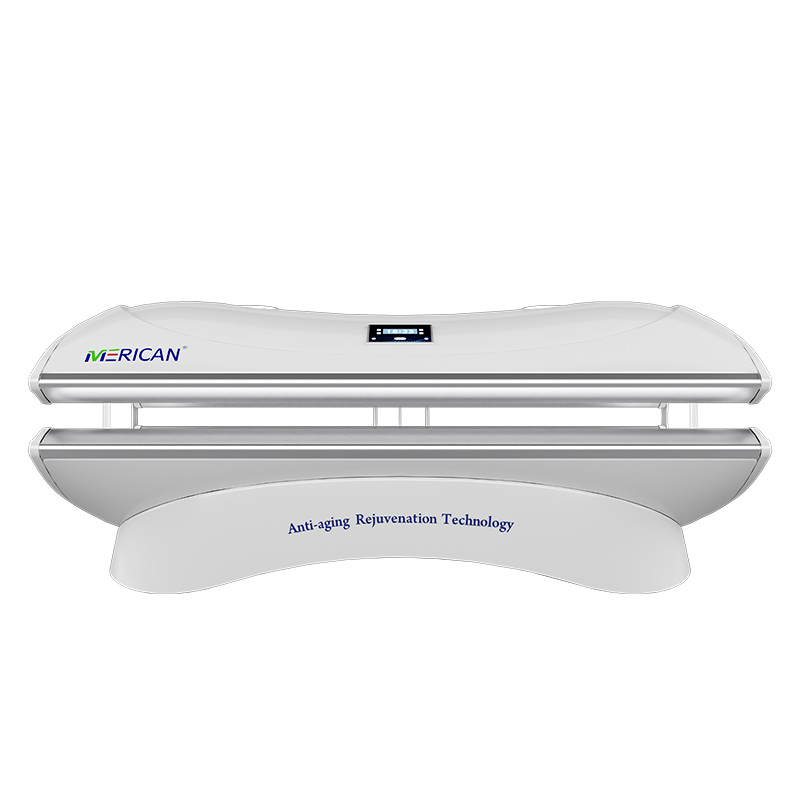
Home Device Selection and Safe Use
With FDA approval for various home devices, proper selection and use are crucial:
Key Points for Device Selection:
- Wavelength Verification: Choose devices that clearly specify the wavelength (على سبيل المثال, 660nm ±10nm).
- Appropriate Power: Home device power density should be between 10-100 MW/CM².
- Irradiation Area: Select a panel size appropriate for the wound.
- Safety Certification: Look for FDA registration or CE marking.
Seven-Step Home Use Protocol:
- Assess Suitability: Use only for clean, minor wounds with no signs of infection.
- Thorough Cleaning: Clean the wound and surrounding skin with saline or a mild disinfectant.
- Device Preparation: Clean the irradiation head; wear protective goggles if the device lacks automatic protection.
- Position and Irradiate: Maintain a distance of 5-15 cm from the skin, ensuring light shines perpendicularly on the wound.
- Time Control: 5-15 دقائق لكل جلسة, not exceeding the device manual’s recommendations.
- Frequency Management: 1-2 times daily; more frequent during the acute phase is acceptable.
- Observe and Record: Document wound changes; take weekly comparison photos.
Chapter 5: Cutting-Edge Research and Future Directions
Personalized Phototherapy Protocols
Latest research focuses on customizing phototherapy based on the wound microenvironment:
- Inflammation Level Detection: Assess inflammation levels via biomarkers to adjust the red/near-infrared light ratio.
- Real-Time Feedback Systems: Develop intelligent phototherapy devices that monitor tissue oxygenation and pH changes.
- Optimized Combination Therapies: Synergistic application with negative pressure wound therapy, growth factors, and stem cell treatments.
New Discoveries in Mechanism Research
Post-2020 studies have revealed deeper mechanisms:
- Mitochondrial Transfer: Phototherapy promotes mitochondrial transfer between cells, enhancing overall tissue repair capacity.
- Epigenetic Regulation: Influences DNA methylation and histone modification, providing long-term regulation of repair gene expression.
- Microbiome Modulation: Specific wavelengths can selectively inhibit drug-resistant bacteria like Staphylococcus aureus while promoting beneficial bacteria growth.
Future Application Prospects
- Wearable Phototherapy Devices: Flexible LED patches for continuous low-dose irradiation.
- Photosensitizer-Enhanced Therapy: Topical application of photosensitizers to increase specific cells’ responsiveness to light.
- Home-Hospital Integrated Systems: Home device data synced with medical teams for remote monitoring and adjustment.
Chapter 6: Common Misconceptions and Safety Notes
Clarifying Five Common Misconceptions
- “Higher Intensity is Better”: Photobiomodulation follows a biphasic dose response; too low is ineffective, too high is inhibitory—there is an “optimal therapeutic window.”
- “It Can Replace All Traditional Care”: Phototherapy is an adjunct, not a replacement for foundational care like debridement and infection control.
- “Immediate Results”: Typically requires 3-5 sessions before effects begin to show; chronic wounds may take weeks.
- “All Devices Are the Same”: Differences in wavelength accuracy, output stability, and irradiation uniformity significantly impact efficacy.
- “It Can Treat Any Wound”: Not suitable for ischemic or malignant wounds; may be harmful.
Safety Warnings and Contraindications
موانع مطلقة:
- Photosensitive skin diseases (على سبيل المثال, porphyria).
- Use of photosensitizing medications (some antibiotics, مدرات البول, إلخ.).
- Undiagnosed skin lesions.
- Direct eye exposure (can cause retinal damage).
Relative Contraindications (Require Physician Evaluation):
- Thyroid disorders (neck irradiation may affect thyroid function).
- Bleeding disorders or use of anticoagulants.
- History of epilepsy (specific light frequencies may trigger episodes).
- الحمل (abdominal area irradiation).
Adverse Reaction Monitoring:
- تقريبًا 2-5% of users may experience temporary redness or dryness.
- Very few reports of headache or nausea, usually related to overuse.
- Discontinue immediately and consult a doctor if any abnormal reactions occur.
خاتمة: The Rational Position of Phototherapy in Wound Management
Red light therapy represents a paradigm shift in wound care from passive observation to active modulation. It does not perform miracles but accelerates the natural healing process by optimizing the body’s inherent repair capabilities. Existing evidence strongly supports its role as an adjunct to standard wound care, particularly for chronic, hard-to-heal wounds.
For patients considering red light therapy, the following steps are recommended:
- Professional Assessment: أولاً, have a wound care specialist evaluate the wound type and suitability.
- Set Realistic Expectations: Understand its adjunctive role and expected time to effect.
- اختر الجهاز المناسب: Select medical-grade or home devices based on wound characteristics.
- Adhere to Standardized Use: Strictly follow treatment parameters and frequency.
- Integrate Comprehensive Care: Combine with nutritional support, pressure relief, and other holistic care measures.
As research deepens and technology advances, red light therapy is poised to evolve from its current adjunctive role into a core component of personalized wound management protocols. في المستقبل, we may see each wound receiving a customized “light prescription” based on its molecular profile—a fascinating prospect at the intersection of regenerative medicine and precision healthcare.