Bei der Erhaltung der Gelenkgesundheit geht es nicht nur darum, Schmerzen zu vermeiden – es geht darum, den gesamten Körper so zu bewegen, wie er sollte, So lange wie möglich. Egal, ob Sie im Teenageralter sind oder kurz vor den Sechzigern stehen, Die Art und Weise, wie Sie Ihre Gelenke heute behandeln, wird sich direkt auf Ihre Mobilität von morgen auswirken.
Dieser Leitfaden soll Ihnen helfen zu verstehen, wie sich Ihre Gelenkgesundheit im Laufe der Zeit entwickelt, und was Sie in jeder Lebensphase tun können, um einen reibungslosen Ablauf zu gewährleisten.
Gelenkgesundheit verstehen
Gelenke sind die strukturellen Verbindungen zwischen Knochen, die Bewegung ermöglichen, Stöße absorbieren, und die Integrität des Skeletts aufrechtzuerhalten. Gesunde Gelenke unterstützen alles, vom Gehen und Laufen bis zum Heben und Strecken.
Zu den gängigen Gelenktypen gehören::
- Scharnier (Knie, Ellenbogen)
- Kugelgelenk (Hüften, Schultern)
- Gleitgelenke (Handgelenke, Knöchel)

Die Erhaltung der Gelenkgesundheit ist nicht nur für die Beweglichkeit, sondern auch für die Vorbeugung chronischer Schmerzen von entscheidender Bedeutung, funktionelle Einschränkungen, und degenerative Erkrankungen, wie zum Beispiel:
- Arthrose: Eine degenerative Gelenkerkrankung, bei der der Knorpel mit der Zeit verschleißt, was zu Steifheit und Schmerzen führt.
- Rheumatoide Arthritis: Eine Autoimmunerkrankung, die eine chronische Gelenkentzündung verursacht, Betroffen sind häufig Hände und Füße.
- Schleimbeutelentzündung: Entzündung der mit Flüssigkeit gefüllten Säcke (Schleimbeutel) die Gelenke abfedern, meist aufgrund von Überbeanspruchung.
- Sehnenentzündung: Schwellung der Sehnen durch wiederholte Belastung oder Verletzung.
Nach Angaben der Zentren für Krankheitskontrolle und Prävention (CDC), fast 54 Millionen Erwachsene in den USA. an irgendeiner Form von Arthritis leiden, eine der Hauptursachen für Gelenkschmerzen und Behinderungen.
Wichtig, Gelenkgesundheitsprobleme sind nicht auf ältere Erwachsene beschränkt. Bei Kindern und jungen Erwachsenen können aufgrund von Sportverletzungen oder angeborenen Erkrankungen Gelenkprobleme auftreten, Bei Personen mittleren Alters kann es hingegen zu ersten Anzeichen einer Gelenkdegeneration kommen.
Wie sich die Gesundheit der Gelenke mit dem Alter verändert

Lassen Sie uns durchgehen, wie sich die Gelenke mit jeder Lebensphase verändern und was Sie tun können, um der Zeit immer einen Schritt voraus zu sein.
Kinder und Jugendliche (0–20)
In diesem Stadium, Gelenke sind im Allgemeinen flexibel und belastbar. Jedoch, Wachstumsschübe und Hochleistungssportarten können sich entwickelnde Strukturen belasten. Aktive Kinder neigen zu Verletzungen durch Überbeanspruchung, wie Osgood-Schlatter-Krankheit. Das Erlernen der richtigen Körperhaltung und die Förderung von Dehnübungen können hier einen echten Unterschied machen.
Erwachsene im Alter von 20 bis 40 Jahren
Hier beginnen viele Leute zu fragen, „Kann man mit 20 Arthritis bekommen??„Die Antwort lautet „Ja“ – und es hängt oft mit sich wiederholenden Bewegungen oder alten Sportverletzungen zusammen. Fügen Sie einen Schreibtischjob hinzu, mangelnde Mobilität, und schlechte Kniesitzposition, und der perfekte Sturm braut sich zusammen.
Wenn Sie jemals Knieschmerzen bei Kniebeugen verspürt haben, Es kann mehr als nur Muskelkater sein. Schlechte Ausrichtung, Muskelungleichgewichte, und eine schwache Hüftunterstützung kann übermäßigen Druck auf die Gelenke ausüben.
Mittelalter und darüber hinaus (50+)
Dies ist der Zeitpunkt, an dem die Menschen beginnen, Steifheit zu bemerken, eingeschränkter Bewegungsbereich, oder sogar hörbare Klicks aus ihren Gelenken. Während eine gewisse Degeneration natürlich ist, Viele altersbedingte Gelenkbeschwerden sind auf Inaktivität zurückzuführen, nicht alleine altern.
| Altersgruppe | Gemeinsame gemeinsame Merkmale | Typische Änderungen | Risikofaktoren | Empfohlene Aktionen |
| Teenager & 20S | Hohe Mobilität, starker Knorpel | Sportverletzungen, frühe Anzeichen einer Überbeanspruchung | Wirkungsvolle Aktivitäten, schlechte Technik | Lernen Sie die richtige Form; Vermeiden Sie eine Kniesitzposition; gelenkunterstützende Muskulatur aufbauen |
| 30S | Beginn des Knorpelverschleißes | Gelegentliche Knieschmerzen bei Kniebeugen, Steifheit | Sitzender Lebensstil, Gewichtszunahme | Stärke einbauen; Flexibilitätsroutinen; ein gesundes Gewicht halten |
| 40S | Frühe Abnutzungserscheinungen kommen häufiger vor | Reduzierte Schmierung, Gelenkdichtheit | Stress, sich wiederholende Bewegung, leichte Verletzungen | Bleiben Sie aktiv; Dehnen Sie sich täglich; Dazu gehören entzündungshemmende Lebensmittel |
| 50S | Spürbare Gelenkbeschwerden | Knorpelverdünnung, langsamere Erholung | Hormonelle Veränderungen, vergangene Verletzungen | Nutzen Sie gelenkschonende Übungen (Baden); Achten Sie auf frühe Arthritis-Symptome |
| 60S & über | Verminderte Flexibilität und Verengung des Gelenkraums | Arthrose, eingeschränkte Mobilität | Altersbedingte Degeneration | Erwägen Sie eine Physiotherapie; Vermeiden Sie längere statische Körperhaltungen |
Tägliche Strategien, um Ihre Gelenke in jedem Alter gesund zu halten

Alltagsgewohnheiten prägen die Gesundheit Ihrer Gelenke mehr als Sie vielleicht denken. Hier erfahren Sie, wie Sie einen Tagesablauf aufbauen, der schmerzfreie Bewegungen unterstützt.
Gelenkschonende Übungen und Bewegungsgewohnheiten
Gelenkschonendes Training bedeutet, Workouts zu wählen, die stärken, ohne zu überlasten.
- Versuchen Sie es mit Wassergymnastik, Yoga, oder Widerstandsbänder.
- Vermeiden Sie anstrengende Aktivitäten, wenn Sie bereits Beschwerden verspüren.
- Ignorieren Sie Schmerzen nicht – Knieschmerzen bei Kniebeugen sollten nicht als „normal“ abgetan werden.
Durch Dehnen werden die Flexibilität und die Gelenkschmierung verbessert. Schon fünf Minuten dynamisches Dehnen am Tag können die langfristige Mobilität unterstützen.
Sitzpositionen für die Gesundheit von Gelenken und Knien
Eine schlechte Körperhaltung wirkt sich nicht nur auf Ihren Rücken aus, sondern auch auf Ihre Kniesitzposition, deine Hüften, und sogar deine Knöchel.
- Sitzen Sie mit den Knien im 90-Grad-Winkel und den Füßen flach.
- Verwenden Sie bei Bedarf eine Fußstütze, um diese Position zu stützen.
- Ändern Sie alle 30–45 Minuten die Position, um Gelenksteifheit zu vermeiden.

Ernährung und Nahrungsergänzungsmittel, die zum Schutz der Gelenke beitragen
Was Sie essen, wirkt sich direkt auf die Gelenkfunktion aus. Eine entzündungshemmende Ernährung unterstützt den Knorpel und reduziert oxidativen Stress.
- Omega-3-Fettsäuren (Lachs, Leinsamen)
- Vitamin D & Kalzium (wesentlich für die Knochen-Gelenk-Schnittstelle)
- Glucosamin und Chondroitin (Nahrungsergänzungsmittel mit einigen Hinweisen auf Linderung)
Auch die Flüssigkeitszufuhr ist wichtig. Synovialflüssigkeit, das Ihre Gelenke schmiert, besteht größtenteils aus Wasser. Eine ausreichende Flüssigkeitszufuhr sorgt im wahrsten Sinne des Wortes dafür, dass alles reibungslos läuft.
Lebensstilfaktoren
- Schlafen: Während Sie schlafen, repariert Ihr Körper Gewebe – einschließlich Gelenkknorpel.
- Gewicht: Übermäßiges Körpergewicht erhöht die Druckkräfte auf die Gelenke – insbesondere die Knie und Hüften.
- Stress: Chronische Verspannungen führen zu Muskelsteifheit und schlechten Bewegungsmustern.
Wenden Sie eine vorbeugende Gelenkpflege an
Wenden Sie beim Heben die richtigen Techniken an, Entscheiden Sie sich für gelenkunterstützendes Schuhwerk, und erwägen Sie die Verwendung einer Zahnspange bei Aktivitäten mit hoher Belastung. Kalte oder warme Kompressen können helfen, die Beschwerden nach körperlicher Anstrengung zu lindern.
Wirksame Behandlungen und Therapien für die Gesundheit der Gelenke
Das frühzeitige Erkennen von Problemen kann Ihnen jahrelange Beschwerden ersparen. Der Schlüssel liegt darin, zu wissen, auf welche Symptome man achten muss und wann es Zeit ist, etwas dagegen zu unternehmen.
Die Symptome erfordern Aufmerksamkeit
- Anhaltende Steifheit, vor allem morgens
- Klickende oder knallende Geräusche, die neu und häufig sind
- Schwellung oder Wärme um ein Gelenk herum
- Verlust der Bewegungsfreiheit
- Schmerzen während oder nach bestimmten Aktivitäten – wie Knieschmerzen bei Kniebeugen
Behandlungen und Therapien für die Gesundheit der Gelenke
Um die Gesundheit der Gelenke langfristig zu erhalten, ist häufig eine Kombination aus medizinischen Eingriffen und gezielten Lebensstiltherapien erforderlich.
| Behandlungstyp | Geeignet für | Vorteile | Vorsichtsmaßnahmen / Notizen |
| Physiotherapie | Leichte bis mittelschwere Funktionsstörung | Stärkt die Stützmuskulatur, verbessert die Reichweite | Muss konsequent sein und von Profis geleitet werden |
| NSAIDS | Entzündlicher Schmerz | Schnelle Linderung der Symptome | Nicht für den Dauergebrauch ohne Aufsicht geeignet |
| Hyaluronsäure-Injektion | Knie-Arthrose | Verbessert die Gelenkschmierung | Möglicherweise sind mehrere Sitzungen erforderlich |
| Kortikosteroid-Injektion | Schwerer Entzündungsschub | Reduziert Schwellungen schnell | Kann bei übermäßigem Gebrauch den Knorpel schwächen |
| Gelenkersatzoperation | Arthritis im Endstadium | Stellt die Mobilität wieder her | Erfordert eine Reha; für bestimmte Fälle geeignet |
Kann Rotlichttherapie bei Gelenkschmerzen helfen??

Integrierende Rotlichttherapie (RLT) Die Integration in Ihre Gelenkgesundheitsroutine bietet eine wissenschaftlich fundierte Lösung, nicht-invasive Option, die zu Hause oder im klinischen Umfeld eingesetzt werden kann. Hier ist ein tieferer Einblick:
Wie es funktioniert
Die Rotlichttherapie strahlt rotes und naheinfrarotes Licht aus (630–850 nm) zur Stimulierung der Zellaktivität im Gelenkgewebe, Förderung der Reparatur und Linderung von Schmerzen.
- Verbessert die mitochondriale ATP-Produktion im Knorpel und den umgebenden Zellen
- Reduziert Entzündungen durch Senkung entzündungsfördernder Zytokine
- Erhöht die Durchblutung und die Kollagensynthese und unterstützt so die Knorpelerhaltung
- Beschleunigt die Reparatur von Mikrogewebe in Sehnen und Bändern rund um die Gelenke
Vorteile für die Gesundheit der Gelenke
- Arthrose & rheumatoide Arthritis: Klinische Beweise belegen eine signifikante Verringerung von Schmerzen und Steifheit.
- Gelenkschmerzen nach dem Training: RLT hat sich als wirksam bei der Beschleunigung der Genesung erwiesen, indem es Entzündungsmarker senkt.
- Weichteilverletzungen: Sehnenentzündung, Schleimbeutelentzündung, und kleine Belastungen bessern sich bei regelmäßiger Anwendung.
- Vorbeugende Wartung: Regelmäßige Sitzungen können den oxidativen Stress in den Gelenken reduzieren, Verlangsamung der Degeneration.
Eine klinische Studie fanden heraus, dass die Therapie mit rotem und infrarotem Licht die Schmerzen bei Knie-Arthrose um ein Vielfaches reduzierte 50%, mit spürbaren Funktionsverbesserungen.
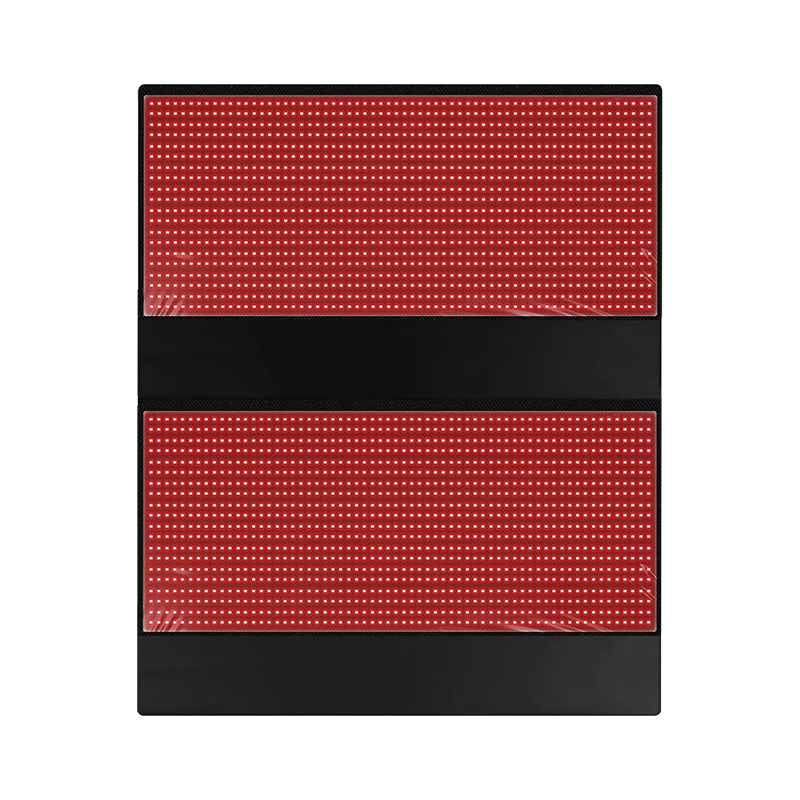
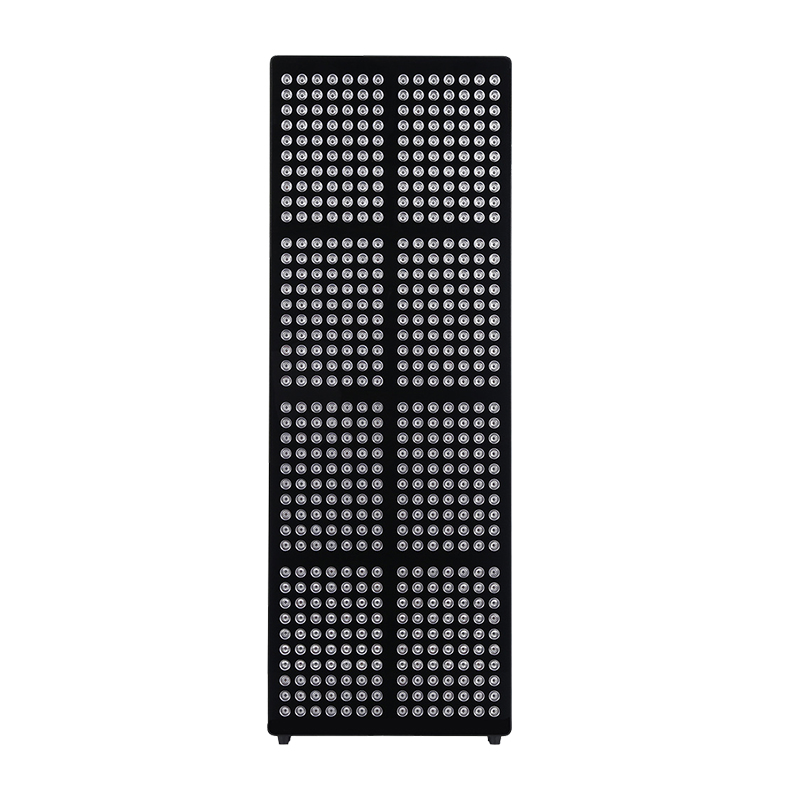
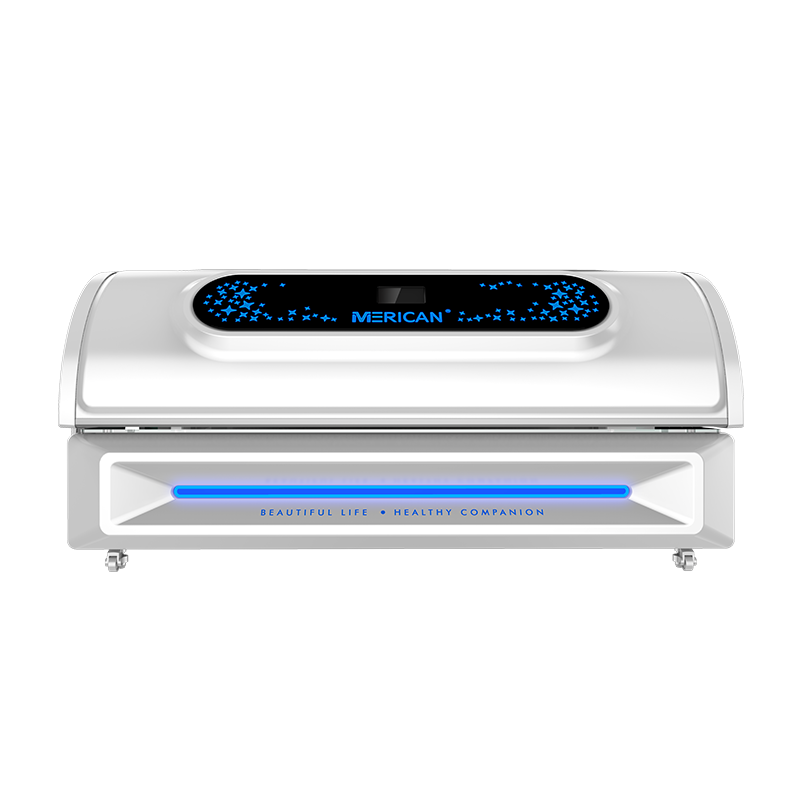
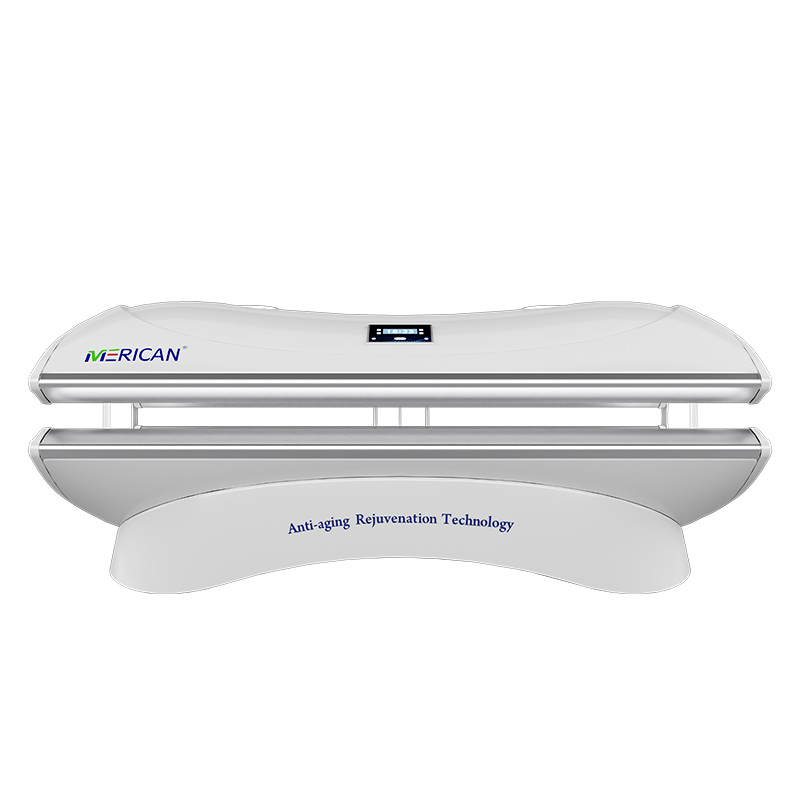
Empfohlene Merican RLT-Geräte
Merican bietet robuste Geräte in klinischer Qualität – jedes mit von der FDA zugelassenen Wellenlängen 660 nm und 850 nm. Alle Modelle sind auf der offiziellen Website von Merican aufgeführt:
Entdecken Sie noch heute die Rotlichttherapielösungen von Merican und machen Sie den ersten Schritt in Richtung einer langfristigen Therapie, Medikamentenfreie Linderung von Gelenkschmerzen.
FAQs:
Was ist die beste Sitzposition für die Kniegesundheit??
Sitzen Sie mit den Knien an 90 Grad, Füße flach, und vermeiden Sie längere Positionen im Schneidersitz.
Wie lindert man Gelenkschmerzen??
Verwenden Sie Physiotherapie, Rotlichttherapie, NSAIDS, Gewichtskontrolle, und Übungen mit geringer Belastung zur Behandlung von Gelenkbeschwerden.
Welches Vitamin ist das beste gegen steife Gelenke??
Vitamin D unterstützt die Gelenkflexibilität und reduziert Entzündungen in Knorpel und Knochen.
Wie lange werden Gelenkschmerzen anhalten??
Die Dauer variiert – akute Schmerzen dauern Tage bis Wochen; Chronische Gelenkschmerzen können über Monate anhalten oder eine kontinuierliche Behandlung erfordern.