Épilepsie affecte plus de 50 millions de personnes dans le monde, et environ un tiers d'entre eux souffrent encore de crises incontrôlées malgré les médicaments modernes.. La quête du non-pharmacologique, les options non invasives se sont donc intensifiées.
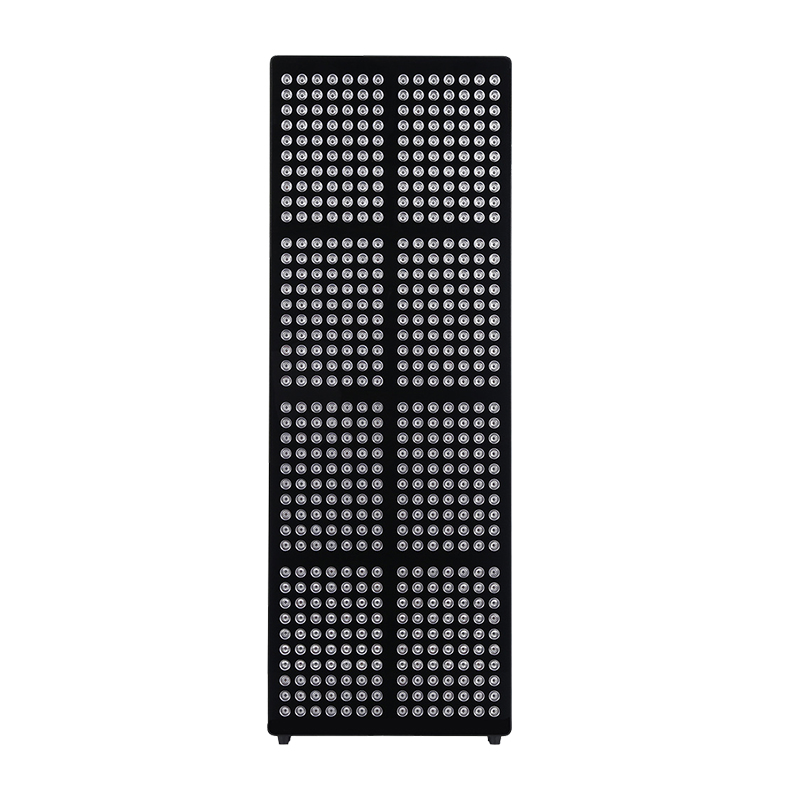
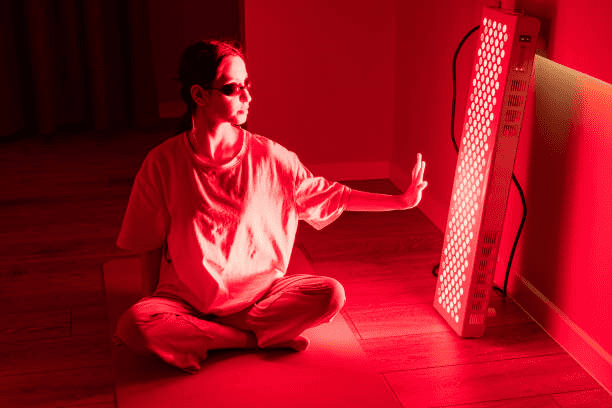
Thérapie par la lumière rouge (RLT)-également appelée photobiomodulation-délivre des photons rouges ou proches infrarouges de faible intensité aux tissus, déclenchant une cascade d’effets biochimiques qui stimulent l’énergie cellulaire, atténuer le stress oxydatif, et moduler l'inflammation.
Au cours de la dernière décennie, les neuroscientifiques ont commencé à poser une question provocatrice: Ces mêmes mécanismes pourraient-ils se traduire par des crises moins nombreuses ou plus légères? Les premières données indiquent « peut-être,» et ce potentiel justifie une étude approfondie, regard équilibré sur les promesses et les pièges.
L'épilepsie en contexte
Espèces, déclencheurs & fardeau
- L'épilepsie n'est pas une maladie mais un spectre, focale englobante, généralisé, génétique, métabolique, et syndromes liés aux traumatismes. Chaque sous-type reflète différents dysfonctionnements des circuits neuronaux, pourtant, tous partagent la marque d'une anormalité, décharges électriques synchrones. Ces décharges peuvent se manifester par des sorts de regard fixe, secousses myocloniques, ou convulsions durant plusieurs minutes, souvent suivi de fatigue et de confusion.
- Les déclencheurs varient considérablement
Manque de sommeil, alcool, stresser, changements hormonaux, infection, et des stimuli visuels (Par exemple, lumières stroboscopiques) sont des précipitants classiques. L'épilepsie photosensible, un sous-type dans lequel la lumière ou des motifs provoquent des crises, représente environ 3 % de cas, principalement chez les adolescents.
- L’impact sur la qualité de vie est profond
Au-delà du danger physique, l'épilepsie restreint les privilèges de conduire, possibilités d'emploi, et participation sociale, tout en augmentant les risques de dépression et de mort subite et inattendue en cas d'épilepsie (SUDEP).
Thérapies standards & leurs limites
- Médicaments anti-épileptiques (ASM) rester en première ligne.
Ils ciblent le sodium, calcium, ou canaux GABAergiques, encore à propos 30 % des patients développent une épilepsie pharmacorésistante (DR).
- Options chirurgicales et basées sur des appareils : chirurgie résective, stimulation du nerf vague, neurostimulation réactive, et stimulation cérébrale profonde – offrent un soulagement à certains patients mais ont un coût, risque chirurgical, et problèmes de disponibilité.
- Les stratégies de style de vie telles que les régimes cétogènes ou la gestion du stress aident certains, mais pas tous.. Dans cette lacune thérapeutique, l’intérêt pour les modalités complémentaires comme le RLT a augmenté.
Voies biologiques reliant le RLT au contrôle des crises

Résilience mitochondriale
- Le dysfonctionnement mitochondrial est un facteur connu d’épilepsie.
Une production altérée d'ATP abaisse le seuil de saisie en déstabilisant les gradients ioniques. Des études sur des modèles murins d'épilepsie du lobe temporal montrent que le NIR (810 nm) les séances restaurent l'ATP et réduisent les durées après décharge.
- RLT remodèle la flexibilité métabolique.
Une phosphorylation oxydative améliorée augmente l'endurance neuronale pendant les périodes d'hyperexcitabilité, potentiellement réduisant la durée et la gravité des crises.
Neuroinflammation & gliale
- Les crises induisent une activation microgliale et une libération de cytokines pro-inflammatoires (IL-1β, TNF-α). RLT régule négativement ces cytokines tout en régulant positivement l'IL-10 et le BDNF, favoriser un environnement réparateur.
- Régulation des astrocytes
En modulant les transporteurs d'aquaporine-4 et de glutamate, Le RLT peut restaurer le tampon potassique extracellulaire, un autre mécanisme anti-épileptique.
Modulation des canaux ioniques
- Des travaux in vitro récents montrent que la lumière rouge/NIR modifie la cinétique de déclenchement des canaux calciques et sodiques voltage-dépendants, relever les seuils de dépolarisation. UN 2024 une revue a souligné la capacité du PBM à moduler les cascades de phosphorylation des canaux ioniques, impactant directement l'excitabilité.
Les preuves jusqu'à présent: Thérapie par la lumière rouge pour l'épilepsie
Données animales
- Modèles de kainate et de pilocarpine pour rongeurs
Séances NIR répétées (830 nm, 30 J/cm²) diminution de la fréquence des crises spontanées de 45 à 60 % et nombre de neurones hippocampiques préservés.
- Synergie optogénétique
Chez des souris transgéniques exprimant des opsines photosensibles, l'association du PBM avec l'inhibition optogénétique en boucle fermée a été éliminée 80 % des saisies, suggérant un potentiel combinatoire.
Premiers rapports cliniques et de cas
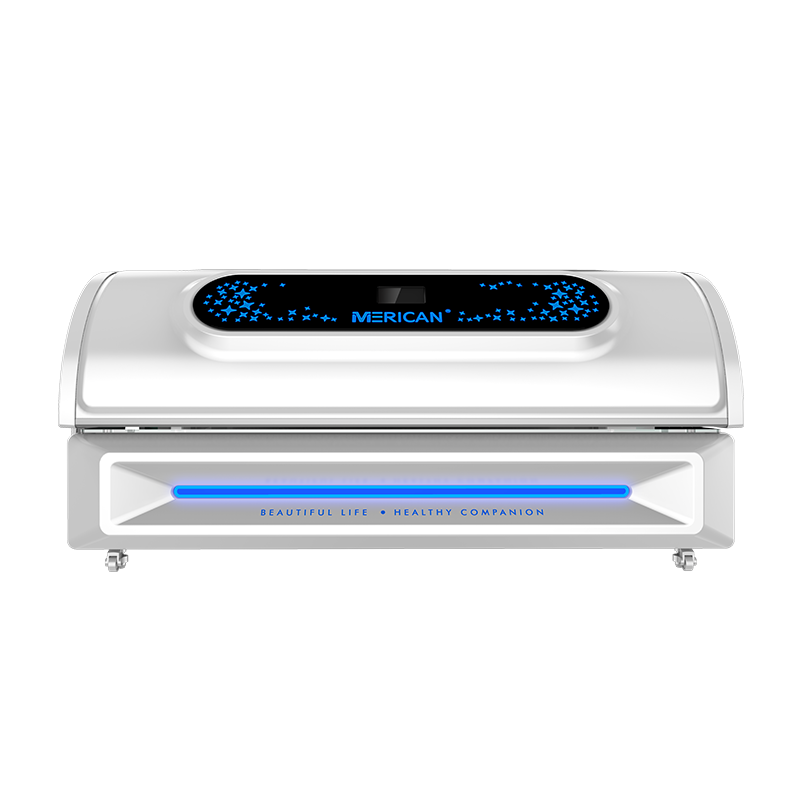
- Pilote ouvert (2023, Australie)
Huit adultes atteints de DRE focale ont reçu un NIR transcrânien (810 nm, 20 minutes, trois fois par semaine). La médiane des crises mensuelles est passée de 12 à 7 sur 12 semaines, avec des scores cognitifs stables ou améliorés. Les effets secondaires se limitaient à une légère chaleur du cuir chevelu.
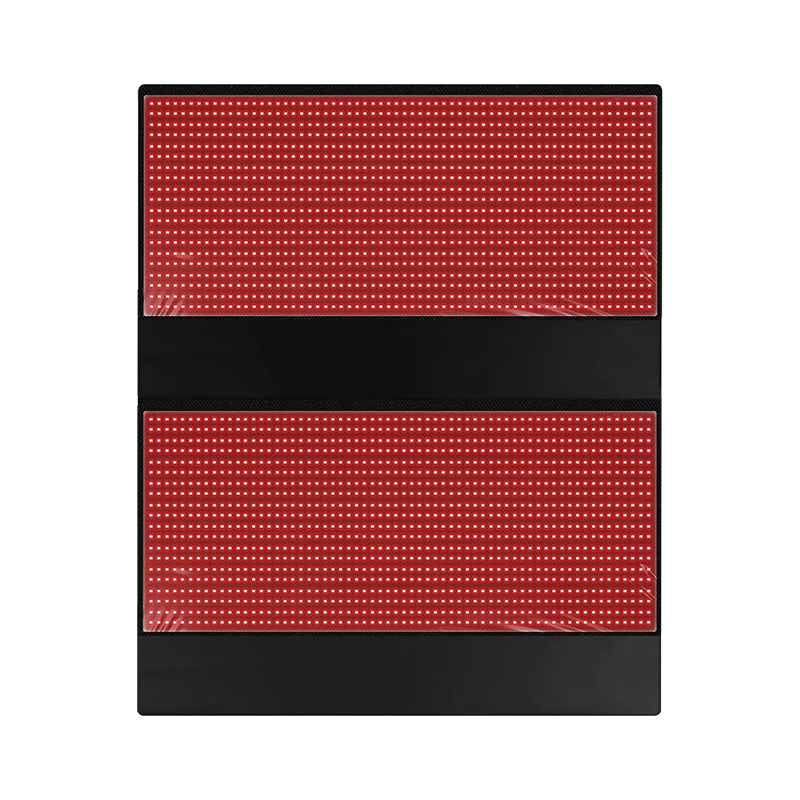
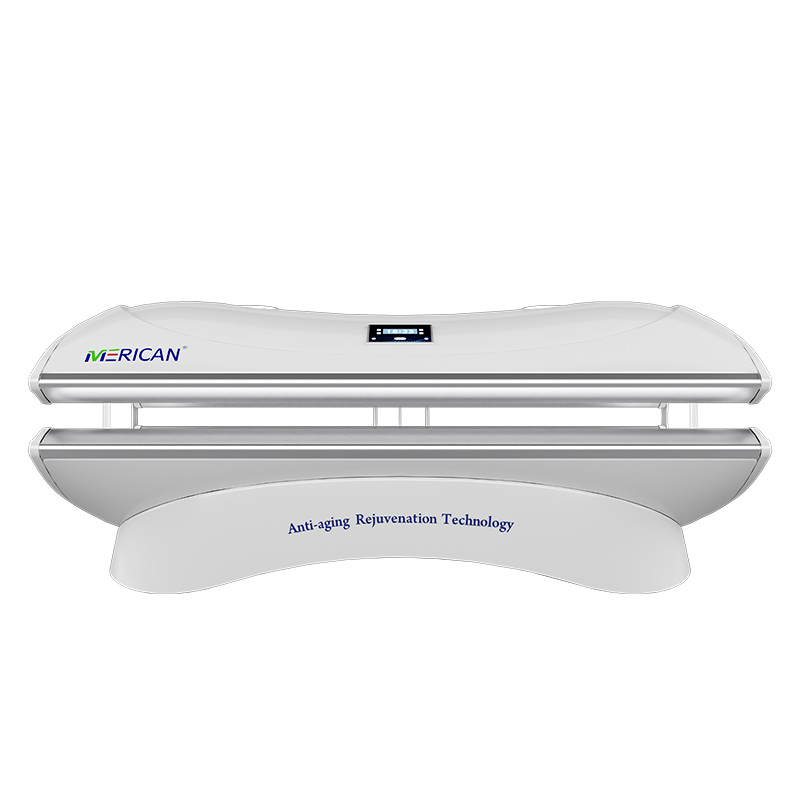
- Audit rétrospectif du Prism Light Pod (2023, USA)
Parmi 22 utilisateurs auto-référents, 41 % reported > 50 % réduction des crises après huit semaines de séances sur tout le corps. Bien que non contrôlé et autodéclaré, les données soulignent le bénéfice perçu par le patient.
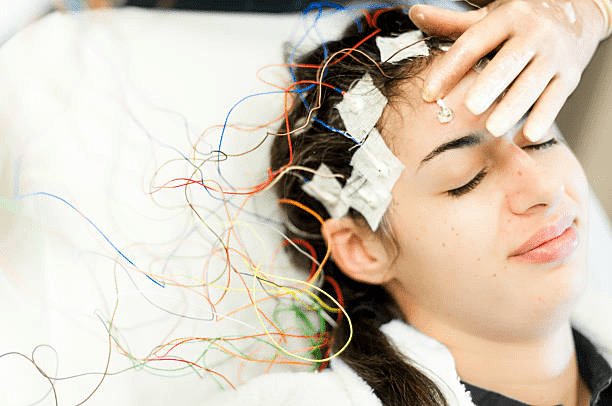
- Des études de faisabilité pédiatrique sont en cours, adapter la conception des casques à des circonférences de tête plus petites et mesurer les changements spectraux EEG plutôt que le nombre de crises comme critères d'évaluation initiaux.
Comment RLT se compare à d’autres outils de neuromodulation
| Métrique | RLT | Stimulation du nerf vague. | Stimulation cérébrale profonde. | tDCS / tMS |
| Caractère invasif | LED/laser non invasif sur le cuir chevelu/la peau | Générateur d'impulsions implantable | Craniotomie pour sondes | Non invasif |
| Mécanisme | Photo-bio-modulation (métabolique, anti-inflammatoire) | Entraînement afférent périphérique | Inhibition du courant au niveau du réseau | Polarisation / magnétique |
| Réduction typique des crises | 30–60 % dans les premières données | 30–50 % (établi) | 40–70 % (en DR) | 20–40 % (variable) |
| Profil défavorable | Douce chaleur, mal de tête rare | Changement de voix, toux | Risque chirurgical | Picotements du cuir chevelu |
Note: Les preuves RLT restent préliminaires par rapport aux modalités de neurostimulation approuvées par la FDA; essais contrôlés randomisés rigoureux (ECR) sont encore nécessaires.
Sécurité & Réponses aux questions sur les risques
Peut thérapie par la lumière rouge provoquer des convulsions?
- Aucune preuve convaincante jusqu'à présent
Contrairement aux lumières stroboscopiques clignotantes (5–30 Hz) connu pour provoquer des crises photosensibles, le RLT thérapeutique émet en continu, lumière non pulsée. Des études animales montrent des convulsions réduction après l'exposition.
- Principe de précaution
Les personnes présentant une photosensibilité sévère devraient quand même commencer par des, séances de faible intensité sous la supervision d'un clinicien et enregistrer toute aura ou événement pendant au moins quatre semaines.
Les lumières LED peuvent-elles provoquer des convulsions?
Oui, mais le contexte compte. Les LED de la maison ou de la scène peuvent scintiller, surtout sur les variateurs, dans la zone dangereuse de 15 à 25 Hz, déclenchant potentiellement des convulsions chez les personnes sensibles. Les circuits de conduite mal régulés sont les coupables habituels.
Les LED de thérapie diffèrent. Les appareils PBM certifiés intègrent des pilotes à courant constant avec scintillement < 1 %. Les utilisateurs doivent vérifier les spécifications du fabricant et, si possible, mesurer le scintillement avec un test de ralenti sur smartphone.
Les meilleures ampoules pour l'épilepsie
Blanc chaud, LED sans scintillement: Choisissez des ampoules explicitement classées « sans scintillement » (< 1 % modulation). Plusieurs marques publient IEEE 1789 rapports de conformité.
Les alternatives halogènes ou incandescentes émettent une lumière constante mais sont progressivement abandonnées pour des raisons énergétiques; ils restent une solution de repli sûre lorsqu'ils sont disponibles.
Les ampoules intelligentes avec température de couleur réglable et courbes de gradation peuvent être programmées pour augmenter ou diminuer lentement, éviter les sauts soudains de luminance. Les ampoules teintées en rouge pour la nuit créent un environnement visuel apaisant et réduisent la suppression de la mélatonine, bénéfique pour le risque de crise lié au manque de sommeil.
Interactions médicamenteuses – Quels médicaments doivent être évités avec la thérapie par la lumière rouge?

Antibiotiques
Tétracyclines (doxycycline, minocycline) et les fluoroquinolones peuvent amplifier les réactions phototoxiques. Les patients doivent soit reporter le RLT, soit couvrir la zone cutanée sous traitement jusqu'à ce que les antibiotiques soient éliminés..
Rétinoïdes
L'isotrétinoïne orale augmente la fragilité cutanée; la combinaison avec une lumière à forte irradiance peut provoquer une dermatite ou une hyperpigmentation.
AINS & diurétiques
Ibuprofène, naproxène, et les thiazidiques provoquent rarement une photosensibilité, mais prolongé, les séances sur tout le corps justifient des schémas de dosage progressifs.
Agents psychotropes
Les phénothiazines et le lithium comportent un risque photosensibilisant bien documenté; un examen de la dose avec un psychiatre est conseillé.
Suppléments à base de plantes
St. Le millepertuis induit des dérivés phototoxiques de l’hypéricine; les utilisateurs doivent suspendre la supplémentation deux semaines avant les cours RLT.
Conclusion
La thérapie par la lumière rouge attire l’attention en tant que traitement complémentaire potentiel de l’épilepsie, avec des premiers résultats prometteurs dans la réduction de l’inflammation, améliorer la fonction mitochondriale, et améliorer la santé du cerveau. Bien que ce ne soit pas un substitut aux médicaments conventionnels contre l’épilepsie, de nombreux chercheurs et patients voient la valeur de sa capacité à soutenir la fonction neurologique et le bien-être général. Alors que d’autres études explorent thérapie par la lumière rouge pour l'épilepsie, il peut offrir une solution efficace, option sans médicament pour aider à gérer les symptômes, surtout lorsqu'il est combiné avec des plans de traitement traditionnels.
Qui dit, la sécurité reste une priorité. Les personnes épileptiques doivent être prudentes avec toute thérapie basée sur la lumière et consulter des professionnels de la santé avant utilisation.. Des questions importantes telles que « La thérapie par la lumière rouge peut-elle provoquer des convulsions ??», "Quels médicaments doivent être évités avec la thérapie par la lumière rouge?» et « Les lumières LED peuvent-elles provoquer des convulsions ??» doit être abordé pour garantir une utilisation appropriée.
Choisir les meilleures ampoules pour l'épilepsie et utiliser des appareils testés cliniquement peuvent aider à minimiser les risques. Avec application responsable, La thérapie par la lumière rouge pourrait devenir un outil précieux dans l’avenir des soins contre l’épilepsie